Don't let ventilation needs limit your day.
The Life2000 Ventilation System may help you:
- Enjoy activities inside and outside your home and live with greater freedom.
- Reduce shortness of breath, fatigue, and discomfort.
- Breathe easier with less effort.

Anna steps out the front door and toward the mailbox. “I love being able to go for walks outside again,” she smiles as she comes back with a package and several letters. Anna has Stage 3 COPD, an obstructive lung disease where the airflow to the lungs is partially blocked. Anna experienced shortness of breath, and even the smallest activities were all but impossible. “I spent most of every day on the couch,” says Anna, “I couldn’t even do simple things like laundry or dishes.” Her husband took over all the household chores. Then, in February, Anna was fitted with wearable ventilation and her life changed.
Now, with wearable open ventilation, Anna can move around her house easily and has been able to go on short walks with her husband.
“I love being able to go for walks outside again”- Anna
Featuring a lightweight, wearable ventilator, it goes where you go, throughout the day and night.
Wearable for true mobility
Several unique features help optimize mobility, comfort, and quality of life:

Detachable
1 lb. detachable ventilator is easy to use and can be secured to a belt, waistband, or cylinder cart with the optional belt clip or pole mount. With three activity settings: rest, moderate activity, and exercise.

Extra long tube
Thin, up-to-50-foot tubing for easy mobility.

Breathe pillows interface
The comfortable and discreet Breathe Pillows Interface lets you talk while in use.

Rechargeable battery
Rechargeable ventilator battery lasts up to 6 hours of normal use.
Wearable ventilation has helped many gain back their freedom and resume their daily activities
Is it right for me?
The Life2000 Ventilation System is cleared by the FDA to provide ventilatory support for individuals who require mechanical ventilation. The Life2000 Ventilation System can help people living with respiratory insufficiency that may result from conditions such as:
- Chronic obstructive pulmonary disease (COPD)
- Neuromuscular conditions such as amyotrophic lateral sclerosis (ALS)
- Restrictive Thoracic Disorders
Ask your doctor
Ask your doctor about the Life2000 Ventilation System if you have respiratory insufficiency and answer “yes” to any of the following questions:
- Are you using supplemental oxygen and still feel a shortness of breath?
- Have you recently had to visit the emergency room or been admitted to the hospital due to respiratory issues?
- Have you recently had abnormal results from a pulmonary function test to arterial gas test?
Insurance Coverage
The Life2000 Ventilation System is covered by Medicare and commercial insurance plans for invasive and noninvasive ventilation. Find a provider call customer service at 1-800-426-4224 or email at [email protected].
How do I obtain a Life2000 Ventilation System?
The Life2000 Ventilation System must be prescribed by your doctor. Consult with your doctor to understand if it is right for you.
How to use
Follow our series of instructional videos for information on how to use the Life2000 Ventilation System:
How to use: Introduction
How to use: Extended Range Configuration
How to use: Stand-Alone Configuration
How to use: Cleaning & Maintenance
How to use: Titration
How to use: Alarms & Troubleshooting
Diseases of respiratory insufficiency
When breathing is impaired, your lungs can’t easily move oxygen into your blood and remove carbon dioxide from your blood (gas exchange). This can cause a low oxygen level or high carbon dioxide level, or both, in your blood. Respiratory insufficiency refers to conditions that reduce your body’s ability to perform gas exchange, including:
- Chronic Obstructive Pulmonary Disease (COPD): a progressive lung disease that includes emphysema and chronic bronchitis. Asthma and rare genetic conditions, such as cystic fibrosis, can also lead to COPD. Interstitial Lung Disease: represents a large group of conditions that scar the alveoli (the air sacs in your lungs) and decrease your lungs’ ability to perform gas exchange.
- Neuromuscular Disease: refers to conditions that affect the nerves and muscles that control breathing. Examples include amyotrophic lateral sclerosis (ALS), often called Lou Gehrig’s disease; muscular dystrophies; and myasthenia gravis. As these conditions progress, loss of nerve function can lead to difficulty in breathing and respiratory insufficiency.
- Restrictive Lung Disease: refers to conditions where lung volumes are limited, reducing the lungs’ ability to fully with with air.
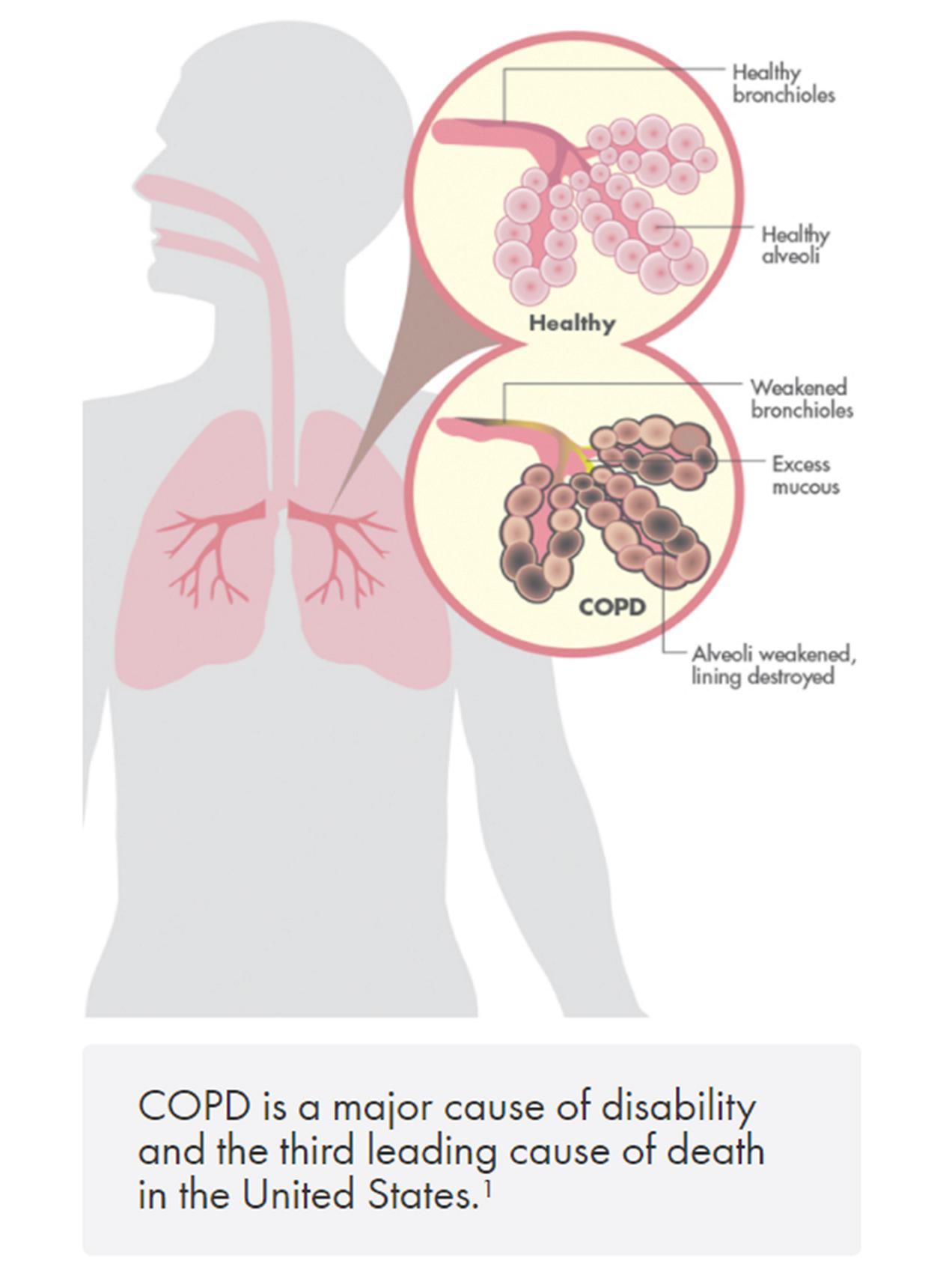
Symptoms of COPD
COPD develops slowly. As the disease becomes worse, symptoms usually become more severe and can limit your ability to do routine activities. Severe COPD may prevent you from doing even basic activities like walking, cooking, or taking care of yourself.
Common signs and symptoms of COPD include
- An ongoing cough or a cough that produces a lot of mucus
- Shortness of breath, especially with minimal physical activity
- Wheezing (a whistling or squeaky sound when you breathe)
- Chest tightness
Diagnosis and treatments
One simple, noninvasive test that your doctor may recommend is called a spirometry test. It measures how much air you exhale and how fast you exhale it. It can also tell how well your lungs deliver oxygen to your blood.
Your doctor may recommend other tests, such as:
- Chest X-Ray or chest CT scan: shows the structures inside your chest and can detect damage or symptoms of respiratory insufficiency
- Arterial blood gas (ABG) test: measures your oxygen level by taking a blood sample from your artery. The result from this test can show how severe your disease is and if you need oxygen therapy
The goals of treatment for respiratory insufficiency include:
Relieving your symptoms | Improving your exercise tolerance (your ability to stay active) | Slowing the progress of the disease
Preventing and treating complications | Improving your overall health

Pulmonary rehabilitation is a program of exercise, education, and support to help you learn to breathe—and function—at the highest level possible. Rehabilitation activities can make a substantial difference in slowing the progression of lung conditions and helping you stay active.

When the oxygen level in your blood becomes low, oxygen therapy may be prescribed. Usually a nasal cannula connected to an oxygen source is worn beneath the nose. At home, this oxygen source may be an oxygen cylinder or an oxygen concentrator. In hospitals, there are oxygen sources readily available.

A mechanical ventilator is a device that makes it easier for you to breathe by providing your lungs with pressurized volumes of air. This treatment may be used if you have trouble breathing on your own or your lungs are having difficulty performing enough gas exchange for your body’s needs.

Medications may relax the muscles around your airways, helping them open wider. These medications may include bronchodilators and inhaled glucocorticosteroids (steroids).

Surgery usually is a last resort for people who have severe symptoms that have not improved with other treatments. Types of surgeries include bullectomy and lung volume reduction surgery. For example, a lung transplant might be an option for people who have very severe COPD.
US-FLC100-230028-v1_Life2000-Patient-Clint-Testimonial_Video.mp4
Clint's Story
US-FLC100-230029-v1_Life2000-Patient-Harry-Testimonial_Video.mp4
Harry's Story
Brian's Story: COPD and the Life2000 Ventilation System
Brian's Story: The Difference with Life2000 Ventilation System
Brian's Story: Life Before and After Life2000 Ventilation System
Brian's Story: Using Life2000 Ventilation System
Find out more.
Contact your Hillrom representative today.





